Join a powerful, unprecedented alliance for better eye health for all.
Join IAPB-
Choose an alternate language here
For World Glaucoma Week, Professor William Morgan on use of a glaucoma drainage device Indonesia…
Glaucoma is the second common cause of blindness in Indonesia, with an estimated 330,000 bilaterally blind patients. The rate is approximately 7/1000 over the age of 50 are blind from glaucoma. The glaucoma prevalence rate is 5 percent with slightly more than half the cases being due to angle closure glaucoma. This tends to be a more aggressive disease and often results in synechial formation before detection. There is often a poor response to medical treatment, which is also expensive and there are problems with compliance, often leading to poorer outcomes. Hence, surgery is more commonly performed. Standard trabeculectomy surgery tends to fail more often than in equivalent European populations, which leaves a large need for glaucoma drainage device implantation.

I set up a very active glaucoma training programme for Indonesian doctors at the Lions Eye Institute. In 2011, working with my PhD student, Virna Oktariana, we designed a novel glaucoma drainage device made from poly methyl methacrylate and silicone tubing, which could be manufactured in Indonesia for 1/10th (US$100 compared to US$1,000) of the standard price. We took this project from animal (fig 1) to human trials in Jakarta with over 100 subjects receiving implants and followed closely for 18 months prior to receiving National approval. The device we called the “Virna Glaucoma Drainage Device” (Virna GDD) is now being manufactured on a large scale cheaply in Jakarta. To-date there have been approximately 1,000 implants with a very active training programme running across the country.

We launched it nationally in Jakarta in June 2019 in alliance with the University of Indonesia, ROHTO (the commercializing company) and the Department of Health. It was the first time that a medical device was designed and commercialized in Indonesia. Our Indonesian colleagues are very pleased about the fact that useful research capacity has been built here. This has made glaucoma drainage device surgery accessible to Indonesia, and because of its accessibility, has facilitated appropriate surgical skills development and training for surgeons. It is having a massive impact upon rates of blindness and is currently the only glaucoma drainage device available in Indonesia due to supply issues and cost constraints. The commercialising firm is looking into exporting the device to other South-East Asian countries. It was part of our plan to make this device cheaply available to other South-East Asian countries, and where possible, teach surgeons in those countries the appropriate technique for insertion and post-op management.
Glaucoma drainage device surgery is technically challenging with particular post-operative management requirements and there is still a large scope for our involvement in teaching young ophthalmologists from various centres across Indonesia. Basically, most of the 330,000 glaucoma blind people in Indonesia would not be blind if they had this surgery and we would like to make this much more accessible, and not just restrict this to Indonesia. There is also a growing need for improved monitoring of glaucoma progression and progression detection given that the prognosis for glaucoma patients has improved but this brings with it demands and needs for better monitoring and treatment adjustment.
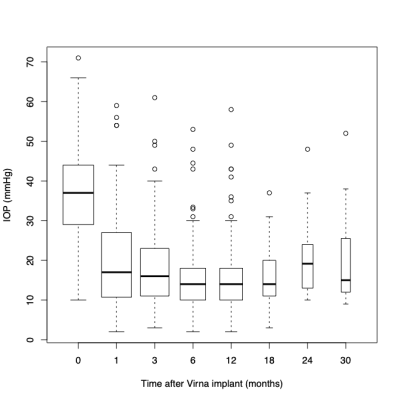
Image on top: Dr Oktariana and I doing animal implants of the original GDD design at Bogor Veterinary University
[vc_row_inner css=”.vc_custom_1583749525922{background-color: #e7ecf3 !important;}”][vc_column_inner width=”1/2″ css=”.vc_custom_1583749682211{padding-left: 15px !important;}”]
[vc_column_text]
The IAPB Global Assembly 2020 (GA2020) programme has several sessions on Glaucoma. If your work is around the topic, do submit an abstract–the sector needs to know!
[/vc_column_text][/vc_column_inner][vc_column_inner width=”1/2″][vc_single_image image=”88500″ img_size=”400×263″][/vc_column_inner][/vc_row_inner][vc_row][vc_column][vc_column_text][/vc_column_text][/vc_row]
[vc_row el_class=”light-row rebelcell prev-blind”][vc_column width=”1/2″ el_class=”cellspace”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][/vc_column][vc_column width=”1/2″ el_class=”cellspace”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][vc_column_text]
[/vc_column_text][vc_separator color=”white”][/vc_column][/vc_row]